It’s four o’clock on a roasting Wednesday last July. I am a resident physician at Yale University, and I am sitting beside my wife, Kristin Budde, who just became an attending physician, also at Yale. We are both opposite our new accountant.
As directed, we have dutifully organized our combined student loans on an Excel spreadsheet. Each row lists a different loan: account number, interest rate and amount. They total just under $300,000.
We have never spoken to an accountant; we’re not from families that have accountants. And 300,000 is an unfathomable amount of dollars. Wide-eyed and disillusioned, we hang on our accountant’s every word and encouragement; it’s the way I’ve seen my patients look as I explain diagnosis and treatment.
Around 5:30, we leave with the clear directive to pay off our student debt ASAP. Our accountant has no confidence in loan forgiveness programs. “Knock down these loans as fast as possible,” he stated with clinical coolness. If we pay off our loans in 10 years, we might be in a good position to, one day, have financial security.
Neither of us questions whether going to medical school was a good investment. Our question is more basic, a more direct extension of the budgetary quandary we’re in now: what did we actually pay for?
“You know, I heard tuition doesn’t even pay for education but that it goes into some kind of slush fund.” I declare, as my fingers curl tightly around the steering wheel, which is sticky with heat. The AC hasn’t kicked in yet.
“That sounds a little dramatic,” my wife says, fiddling with the AC.
There’s a pause.
“N.Y.U. medical students don’t pay tuition anymore.”
“Jealous,” she says. “I thought I was getting a good deal.” She went to medical school in Texas, where tuition is among the lowest in the country.
I mention that Robert Grossman, the dean and CEO of NYU Langone Health, spent over a decade building a $650 million endowment to replace tution. Curious how he did it and whether other schools will follow suit, I decide to go meet Grossman.
I’m sitting on the 15th floor of N.Y.U.’s Langone Medical Center. I’ve taken the train from New Haven to meet Robert Grossman.
When Grossman became the dean and CEO in 2007, the school was hopelessly in the red. Following his appointment, he oversaw what one author called “the most hopeful and positive healthcare stories of our time.”
Under Grossman’s leadership, revenue rose from $2 billion to $10 billion. Research funding more than doubled and, with 1.2 million added square feet of hospital and research space, the total number of employees ballooned from 7,000 to 40,000.
In addition to learning more about academic finances, I want to meet Grossman in person to size him up, to understand why he’d spend 10 years building an endowment to give away tuition. He announced the endowment in 2018 as a “moral imperative,”saying the opportunity cost of student debt crippled young doctors. Critics disagreed, arguing that Grossman’s endowment was no more than a calculated business move to recruit students.
I arrive early and notice that his staff endearingly calls him “Bob.” I’m flipping through a coffee-table book when Grossman rounds the corner. He extends a warm handshake and we walk to his office, an expansive room with a circle of plush sofas.
Grossman agrees to let me ask personal questions, about his family and childhood. He grew up poor, sharing a bedroom with his uncle and brother. During high school, Grossman’s glamorous side-hustles included washing dishes at a local summer camp, a paper route, and cleaning a butcher shop each night. He describes working in Connecticut during the summer and, with a chisel and hammer, scraping the paint off Glen Island Casino’s siding. He still remembers the buzz of pleasure boats as he stood on a ladder for hours tap-tap-tapping away.
“I always saw myself as an underdog,” he says with a charming, toothy grin, “because I was an underdog.”
After medical school, Grossman and his wife (also a physician) raised two children while paying off $12,000 in student debt—a large amount at that time, but a far cry from the $55,000 that the N.Y.U. medical students used to pay each year in tuition.
Tuition has increased exponentially since Grossman was a medical student—more than twice as fast as inflation. Now, physicians graduate with a median $194,000 in student debt. I mention that each year, N.Y.U.’s 450 medical students paid a total of $25 million in tuition.
“So where does this money go?” I ask Grossman.
“Well, where do you think?” he asks, smiling, raising his hands and shrugging shoulders. I think I know what he’s about to say, but I’m surprised when he says it so bluntly.
“It supports unproductive faculty,” he states coolly.
Unproductive faculty, Grossman explains, are people who draw a monthly paycheck, but don’t write grants, teach, or see patients. Tution also funds other expenses, but the vast majority of tuition is not spent educating students.
“Think about it,” Grossman continues, “How many full-time faculty does it take to teach a group of medical students? Twelve or 13?”
I think back to my own medical education and tally up the faculty instructors. Thirteen sounds about right.
Grossman continues: “You only need say 12 or 13 FTEs [FTE is a full-time employee] because there’s one teacher at a time for 150 medical students.”
“Well, you could easily pay that salary with 25 million dollars,” I state the obvious. “N.Y.U.’s annual budget is nine point seven billion—"
“Almost 10 billion,” Grossman corrects me with a grin. He tracks every dollar N.Y.U. makes—from clinical revenue, to research grants, to tution.
“OK,” I say, rolling my hand in the air, “Let’s call it ten billion–ish. So then 24–25 million of that is what? A quarter of a percent?”
“A rounding error.”
“A rounding error.”
We both nod.
It’s easy to get lost in the numbers. Rounding error or not, before Grossman’s endowment, N.Y.U.’s medical students paid $25 million in tuition each year, only a small fraction of which was needed to support their education. I want to know whether tution is equally divorced from educational costs at other schools.
It strikes me as a question for a regulator. Physicians have one of the strongest, most organized lobbies in the U.S. and they carefully regulate medical programs to ensure that future doctors are well-trained and not exploited.
The Liaison Committee on Medical Education (LCME) regulates programs that train U.S. physicians. When a program doesn’t meet the LCME’s 12 standards, a program is placed on probation and might lose its accreditation and ability to graduate medical students.
The final LCME standard concerns student finances. The LCME ensures that schools “minimize the impact of direct educational expenses (i.e., tuition, fees, books, supplies) on medical student indebtedness.”
Curious how this works, I call Robert Hash, of the LCME’s Executive Staff Secretariat. Hash tells me that (in another LCME standard) the LCME ensures that the dean controls the price of tuition and that deans raise philanthropic funds to offset educational costs. For example, Grossman held annual galas explicitly to build his tuition endowment.
I recount Grossman’s assertion that tuition supports unproductive faculty and ask how the LCME ensures that tuition is spent on student education and doesn’t end up in a dean’s discretionary account.
“The schools have to provide documentation of where their funding goes.” Hash told me. “They’re audited just like every other institution that deals with money in the country.”
“So you can see where student tuition is going?”
“Not really. We can see that funds aren’t being diverted into a storehouse somewhere,” he says with a chuckle.
I ask Hash whether they paint tuition dollars red and ensure that tuition is spent educating students. The answer is no. The LCME cannot access this information.
Hash notes that the LCME recognizes and is concerned about medical programs’ lack of financial transparency. Instead of comparing tuition to educational costs, they instead justify the cost of tuition with “indirect measures” like sufficient faculty, clinical and laboratory resources, and classrooms per student.
The LCME can ensure that education quality meets their standards, but they have no visibility into how much medical education actually costs or whether a school spends tuition on student education.
The LCME tasks itself with ensuring that medical programs don’t financially exploit their students. And yet the one financial tidbit that would help them assess this—how education cost compares to tuition—is beyond their grasp. Without knowing what education costs, they focus on education quality.
But education does have a cost. Somewhere, in some office, an actual person is paying actual bills: desks cost concrete amounts of money, electricity costs a known number of dollars, faculty are paid real money in exchange for real services, etc. The cost of educating a medical student ought to be concrete and countable because it is paid for with concrete, countable dollars.
I’m willing to admit that no two schools have precisely the same expenses: real estate costs more at N.Y.U. than it does at the University of North Dakota; group-based curricula cost more than lecture-based curricula. But the fact that tuition ranges from $16,000 to $93,000 per year has to be explained by more than just a real estate market or an educational philosophy. It sounds like a question for an economist.
I call Amitabh Chandra, the director of health policy research at Harvard’s Kennedy School of Government. Chandra explains that, “in any industry—and medicine is no different—the price of the service depends on the cost of producing the service.”
“But!” Chandra emphasizes, “But it also reflects the willingness to pay for that service.” Tuition is part of a basic supply-demand market equilibrium: each school sets its price tag to maximize the amount its officials they think they can get for their product.
“Even if the cost were zero, it is not the case that medical student tuition would be zero.” Chandra continues, “It would be high because people’s willingness to pay for the degree is high.… That’s the harsh economics of pricing.”
In addition to the LCME, I tell Chandra that I also spoke with a representative from the American Association of Medical Colleges who, it appeared, was convinced that medical school finances were impenetrably opaque, that the marginal cost of educating one medical student was in some weird, Borgesian way, uncountable.
Chandra stops me, reminding me that the numbers are all there (i.e., someone pays the bills), but most schools simply don’t spend the effort to sort out their cost structure.
“Why not?” I ask, “That boggles my mind!”
“I think it should. One of the reasons that health care is 20 percent of our GDP is that nobody knows their cost structure and yet everybody thinks that they’re losing money somehow. I think this is the key irresponsibility at the heart of medicine: the inability and unwillingness to learn one’s underlying cost.”
Tuition is skyrocketing because college kids keep lining up to pay whatever price the schools set. The more kids line up, the higher the price.
Each year, only 41 percent of applicants are accepted into medical school. Because demand outstrips supply, medical schools have the economic upper hand and, because lenders invariably approve loans to cover tuition, schools can effectively set the price of tuition to be whatever they want. College kids who don’t like it need not apply—somewhere in the remaining 59 percent, an applicant is willing to pay.
So if a college kid wants to become a doctor, she is forced to give her medical school carte blanche. Schools withdraw.
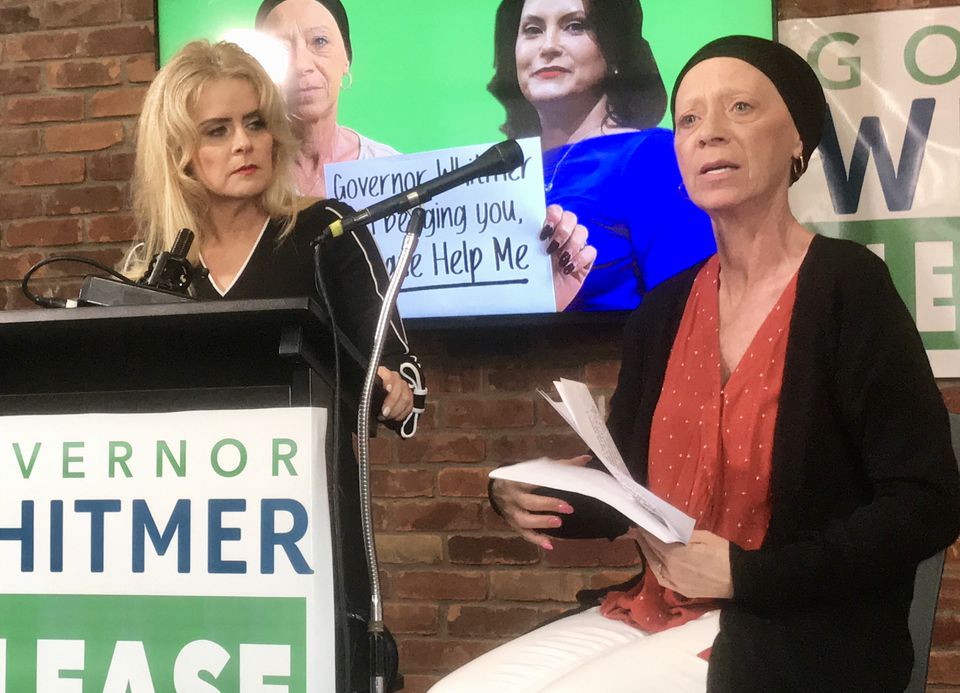
Schools withdraw so much that despite scholarships and cash payments, each year a class of new doctors graduates with a total of $2.6 billion in loans, with a median student debt of $194,000. And no one—not even the regulator tasked with protecting students—can say where this money goes.
It dawns on me that tuition is easy money. If you’re dean of a medical school staring at a deficit, withdrawing progressively larger sums of money from a yet-unknown student is easier than having an uncomfortable conversation with your faculty.
Grossman is a true anomaly. When he became dean/CEO, N.Y.U. Langone Health was running a $150 million annual deficit; hardly a time to build an endowment to fund a $25 million tuition giveaway. Yet, as a self-identified underdog, he wanted to spare his fellow underdog medical students from shouldering N.Y.U.’s budget problems.
Sitting in Grossman’s office, I’m curious whether he’s something of a celebrity genius among academics—or at least among other medical school deans.
“Have you been contacted by other medical schools or other deans or CEOs? You know, for a playbook?” I ask Grossman.
“No. Nothing.”
“Fascinating.” I say, more to myself than to Grossman, trying to make sense of that.
I try a different approach: “A lot of people got on board with the philanthropy at N.Y.U. because they could see you making changes, trimming, as it were. I wonder why other schools don’t try the same thing?” I ask, leaning forward.
“I think that it takes some courage, right? It’s not so easy to do that. It’s easy to say ‘Hey, we’re going to continue inertia.’” Grossman sighs and pauses thoughtfully. “This is a process that took a decade and, a time frame that most medical school deans don’t have.”
I press him on what makes N.Y.U. different.
“Some institutions don’t want to address it.... They don’t view [tuition] as their most important prerogative. They want donors to give money for buildings, bricks and mortar, and—”
“Professorships?” I add to show I’ve been paying attention.
“Professorships, all the usual stuff. The students,” Grossman chuckles, “students are the caboose. These kids....” Grossman pauses pensively, perhaps remembering raising two children while paying his $12,000 debt, “they’re looking a little like I was, but probably worse. So I thought it was really a moral imperative for us to support them in a substantive way.”
A few months later, I’m moonlighting at a local hospital to make some extra money. I just admitted my last patient of the night and am sitting at my computer.
I call my Kristin, who’s at home with our sleeping two-year-old son, and tell her that I can’t decide how to end this story.
“Well, what’s your main point?” she asks, invariably cool, rational.
“Each year, thousands of doctors graduate with debt that has nothing to do with their education. And no one really bothers to sort out where that money goes.”
“Sounds like a stupid system,” she says.
“Does the idea that our debt might have subsized unproductive faculty bother you?”
“Um, yeah,” she says, “I sacrificed much of my youth to be a doctor.”
“What does that have to do with it?”
“I think I imagined that my life would be really glamorous once I was an attending,” she pauses. “We’re fortunate. We have a roof over our head, we can start a family and all that. But we’ve got a crushing amount of student debt and it’s probably going to be a decade before we can see actual daylight.”
“Fair enough—" I try to chime in as my fingers hurry to transcribe what she’s saying.
She continues: “And what’s frustrating is the idea that even though we’ve sacrificed so much already, our debt is an amount of money that schools might not actually need. In order for a school to have a little bit of breathing room on their books, we spend years digging ourselves out of debt? How is that fair?”
“Well, it’s not.”
“And what I worry about is that if this is happening to doctors—if doctors can’t even do something about student loan debt—what hope is there for anyone else?”
Source: https://blogs.scientificamerican.com/observations/why-doctors-are-drowning-in-medical-school-debt/