Your doctor may be playing medical video games at work. That could be good for your health by Edward Baig
Can playing video games be a prescription for good health?
Dr. Zubin Damania thinks so.
Two to three times a week, the UCSF/Stanford-trained internist and founder of the Turntable Health primary care clinic is on his smartphone playing video games.
Damania isn’t seeking a diversion by parachuting into a "Fortnite" battle royale.
“People who are good at video games are actually good at some aspects of clinical medicine.”
Dr. Jacqueline Morano, University of Chicago School of Medicine
Instead, ZDoggMD, as he’s known by his pseudonym as a producer of health care videos and live shows, is among the 400,000 medical professionals practicing the craft of medicine through a series of games from Level Ex, a Chicago video games developer whose titles are specially designed for doctors, med students and other health care providers.
The Level Ex lineup currently consists of a quartet of free games for iOS and Android, with others under development.
There’s Airway Ex targeted to anesthesiologists, Gastro Ex for gastroenterologists, Pulm Ex for pulmonologists and Cardio Ex for cardiologists.
“Having grown up with video games, the idea that you could actually practice a technical skill set and a knowledge-based skill set in medicine while getting the same little burst of happiness and joy and dopamine to use the neurotransmitter from playing a game, it seems to all fit,” Damania says.
Adds Dr. Jacqueline Morano, a neurosurgical anesthesiologist and assistant professor at the University of Chicago School of Medicine, “People who are good at video games are actually good at some aspects of clinical medicine.”
Doctors earn extra credit for playing
The Level Ex games are based on actual and sometimes rare cases that have been submitted by physicians. And however unorthodox it may seem, by playing them doctors can earn CME or continuing medical education credits toward maintaining their licenses.
"It is super important for us to have access to continuing medical education,” Morano says.
The next Xbox is coming: E3 2019: Microsoft unveils Project Scarlett console during Xbox event
The next Star Wars video game: E3 2019: In 'Star Wars Jedi: Fallen Order,' video game you become a Jedi Knight
Level Ex is the brainchild of CEO Sam Glassenberg, whose background in video games (at places such as LucasArts and Microsoft) made him the “black sheep of the family” when he didn’t follow his kin to medical school.
For sure, Level Ex has hired its share of video game developers, but the company also employs full-time MDs and biomedical engineers.
Level Ex also relies on more than 150 physician advisers with pedigrees from Harvard, Stanford, Northwestern and elsewhere who submit cases and ensure the accuracy of the challenges.
To the laymen, the computer-generated graphics look realistic, down to how blood changes color when it mixes with other bodily fluids or how the patient swells or breathes. But with sound effects, music, the use of color and certain controls, there are allowances made for the gaming environment.
Some cases within games exploit augmented reality technology, in which the virtual blends in with your real-life surroundings.
One complex case inside Airway Ex involves a 45-year-old male emergency room patient who has been complaining about a shortness of breath. A large, obstructive supraglottic tumor is discovered. The patient requires intubation and the player must figure out how best to remove the mass.
In a Pulm Ex case based on a real-life incident, a patient is a carpenter who accidentally inhaled a nail. The nail punctured the wall of the trachea. A doctor/player trying to remove the nail in this complex case can consult actual chest X-rays and CT scans.
Doctors trying solve Cardio Ex cases might have to figure out which configurable stents, balloons and atherectomy drills are required to restore the flow of blood to the heart.
The Cardio Ex video game is aimed at cardiologists.
The Cardio Ex video game is aimed at cardiologists. (Photo: Level Ex)
Scoring points and consequences
As part of the various scenarios, players are scored on speed, tissue trauma, loss of blood and, of course, the accuracy of the procedure and whether the patient survives. Doctors can compete against other physicians or themselves. And yes, as with other video games, players can compare their results to the top scores.
The degree of difficulty and challenges get harder as you go. The biggest and most complex cases are where physicians can earn CME credits.
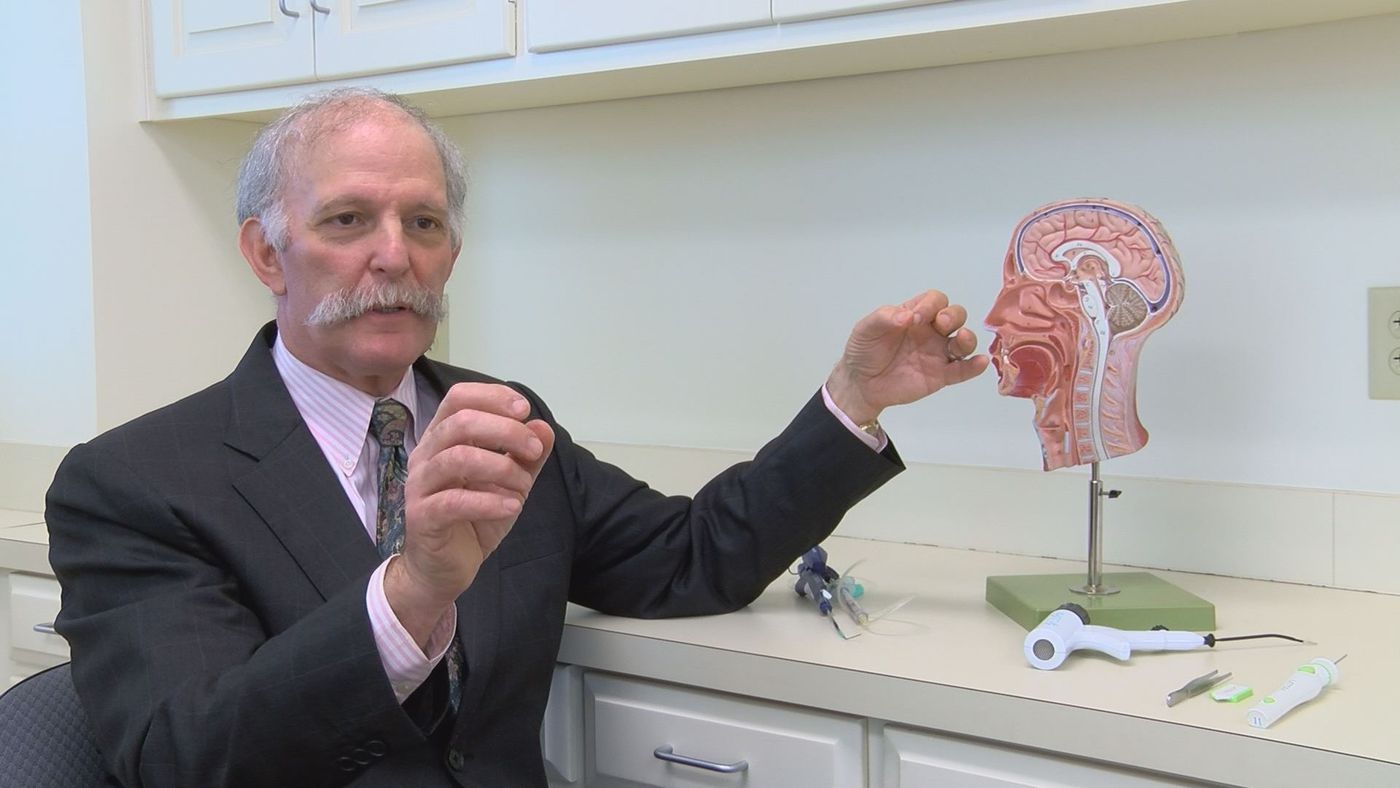
Dr. Eric Gantwerker divides his time between being Level Ex’s vice president and medical director and his medical practice as a pediatric ear, nose and throat surgeon. He jokes that he sometimes tells parents of patients or the patients themselves that he’s perfected his craft playing video games.
“You have to really measure your audience and see how they respond,” he laughs.
Though the free app games are designed for doctors and others in the medical field – and include their share of medical jargon – anyone can play them. If you’re about to have a colonoscopy, you might get a sense of what you’re about to go through by playing, Gantwerker says.
Since Level Ex combines game play and education, the designers must balance the rewards that come with doing well against making it challenging enough to keep players interested.
Losing the game – and the patient
Meanwhile, since Level Ex games are just that – games – they’re meant to be fun, even if the back story to cases may involve real life-and-death situations.
“There’s actually a big discussion in all of the simulation world and even in games about losing a patient and what that effect is on the provider or the person playing the game,” Gantwerker says.
So how does botching procedures and scoring poorly inside the games affect the confidence of a doctor who must confront those real-life cases?
“We give you the opportunity to take on very serious scenarios, but being able to do it in an environment where there's no consequences means you can try different approaches,” Glassenberg says. “One of the best ways to learn is to fail. I would much rather fail on a virtual patient than a live one.”